Treatment is Over, Her Journey Continues
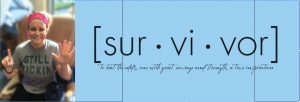
In celebration of Christina Kuzma’s successful fight against breast cancer at the age of 33, Tx:Team brings you the final part of our series to share her experience with physical therapy during treatment.
Everything about cancer was out of Christina’s comfort zone. It turned her world upside down in a moment and put everything that she had lived for on the line: her family and friends, her ambition, her days spent on the lake. What would her life look like a year from now? Before her bilateral mastectomy, Christina couldn’t have imagined how many normal movements would be affected. When she began physical therapy, simply sitting up or lying down was difficult. Christina told herself, “Everyone has just one life, and faces adversity in many ways. So many days I want to curl up and be sick. But that’s a day wasted. I am breathing, and I have a heartbeat, so it’s time to take the energy I do have and do something remarkable with this day. Even if that means something small like smiling at a stranger.” After she was declared cancer-free post-op, she continued to fight – striving to regain the strength and degree of health she had before cancer entered her life.
Christina is all about taking the harder sprint to have an easy marathon. Physical therapy after a grueling 6-hour operation was not easy. She was in a lot of pain completing the simplest of stretches. It was at this time that Christina separated herself from convention. Every day, patients receive opioid medications for their pain. However, Christina is living proof that the positive long-term results of pursuing physical therapy and foregoing opioids outweigh the short-term pain.
When we left off at Christina’s second week of therapy after surgery, she was just becoming strong enough to lift her arms above her head and wash her hair. In her third week post-op, Christina’s physical therapist offered new exercises to up the ante and push her further.
CHRISTINA’S EXERCISES
Throughout the day, she concentrated on her posture, squeezing her shoulder blades to release the tension built up in her chest wall. When she was in the shower and her muscles were more flexible from the heat, she would stand and slide her open palm up the wall. During the “wand exercise” she was on the floor holding a yardstick. She raised her hands above her chest and held the stick in place for as long as she could. This specifically targeted the area from where her lymph nodes were removed. She also practiced putting her arms behind her head in the sit-up position to move her elbows up and down. This exercise would specifically prepare her for the position she would be in weeks later while receiving radiation treatments.
By the end of the fourth week, she regained full range of motion in her arms and resumed the responsibilities of daily life. She was also able to discontinue her Tylenol use. Reaching up for dishes or pantry items was still a struggle, but her pain had subsided. Now, she could get outside every day for a walk- a small win, but a huge improvement. She felt good enough to get back to work. To start, she practiced driving in her neighborhood. Again, she was shocked by how difficult some of those movements were. Looking over her shoulder to change lanes was a slow and careful motion. But by now you know she kept practicing despite the challenge. She even began to coach her three-year old daughter’s soccer team, comfortably bending down to pick up all the soccer balls- incredible.
WHERE IS SHE NOW?
Today, exactly 17 weeks since her surgery in August, Christina is wrapping up radiation therapy. With only one more appo
intment to complete, Christina reflects on her past year, saying: “The one thing I would have done differently is start physical therapy sooner.” Despite her success, she thinks that her body would have been better prepared for the pain and stiffness if she had participated in physical therapy during the weeks leading up to her surgery. Supervised pre-surgical exercises are especially important to post-operation outcomes.
Although her treatment is over, her journey continues. 2018 was not just her year battling cancer, with months of stress, complete exhaustion, pain, and frustration. 2018 was also the year that Christina worked to become a stronger version of herself. One who is vocal about what she knows is good and right for her. One who appreciates the strength it takes to simply lift her arms over her head. One who is so thankful for her health and body providing the opportunity to be outside on a soccer field with her daughter.
2018 was the year that Christina became an advocate for physical therapy as an integral part of breast cancer recovery. Even now, months later, she’s keeping up with her PT appointments. To put it simply, she “Won’t Back Down”. Ultimately, she wants others to know that doctors are receptive to the way you want to heal; talk with them openly. Second, no matter your age or health status, all women need to check their breasts. Early detection saved her life. And she hopes that more people will consider her approach if faced with a similar challenge. Physical therapy is a safe and effective way to heal your body and treat your pain. Prioritize your body’s long-term health.
Our hope is that Christina’s story will impact others for years to come, serving not only as an inspiration for people diagnosed with breast cancer, but for people struggling with chronic pain in any form.


